
Health Services
- Home
- 2020 Recognition
- Departments
- Health Services
Health Services response to the pandemic

Health Services response
The Ambulatory Care Network (ACN) partnered with the Los Angeles Mayor’s Office and the Department of Parks and Recreation to bring medical services directly to homeless persons staying in emergency shelters. Department of Health Services (DHS) employees from ACN’s Mobile Clinic are working with staff from the Department of Mental Health and the Los Angeles Homeless Services Authority to ensure the health and well-being of every shelter resident.
In addition to meeting face-to-face with a medical provider, patients are also provided with connections to additional supportive services. This may involve coordinating with other stakeholders in order to effectively address the individual needs of each person. This model of building sustained relationships with homeless patients works because they see that the DHS team really cares about their health. "Meeting the patients where they're at is half the battle," said Anthony Fedon.
The Mobile Clinic is a tremendous example of how we can use design thinking and Lean methodology to get things done quickly and efficiently. It’s a great example for future DHS projects” said Dr. Kyle Ragins, Director of Urgent Care.

Bedside Energy Boosters & Pocket Programs
Olive View-UCLA Recreation Therapy staff were able to continue providing group programming to behavioral psychiatric inpatient units, despite COVID-19. Staff were extremely resourceful and had to dig deep creatively to adapt programming in order to be compliant with infection control standards and physical distancing guidelines while meeting patients’ interests, abilities and needs. Below are two examples of program adaptations: BEDSIDE ENERGY BOOSTER Program was designed to combat a sedentary lifestyle by providing daily guided meditation, range of motion, and calisthenics modalities from the side of the patient’s bed.
Staff encouraged clients to take ownership in their health in the midst of shut-in orders as well as track daily progress with patients. POCKET PARTIES were designed to combat social isolation and disorientation to time/place/season by celebrating seasonal events. Staff bring the party to the patient by hosting bedside programming for each patient with a “faire” of experiential therapies to incentivize positive social interaction, cultural awareness and social normalcy.

Correctional Health's Staunch Dedication to Serve
As healthcare providers serving a unique patient population, Correctional Health Services (CHS) had many of the same needs as the rest of Department of Health Services (DHS) but challenges unlike any other when the pandemic hit. As tests became available to DHS, CHS was on a mission to test literally thousands of incarcerated patients. Special COVID-19 Teams were assembled and deployed across all jail facilities to conduct oral and nasal swabs, which were executed far more quickly than we could have hoped. Much to their credit, these COVID-19 Teams braved the quarantined units and conducted themselves with speed, efficiency and compassion despite the unknown.
The patients’ fears were quelled as testing became available and survivors were emerging amongst the incarcerated population. In addition to receiving appropriate PPEs and rolling out COVID-19 Teams, the Quality and Patient Safety Department nurses were deployed to assist with an already overburdened system. One nurse, Maria Alejandria, was deployed to Pitchess where she was faced with many tasks; on average she was taking 400+ temperatures daily! These amazing staff members demonstrated a profound sense of duty by placing themselves on the front lines in the midst of incredible uncertainty.

Bedside Energy Boosters & Pocket Programs
In response to the coronavirus pandemic, the Los Angeles County Department of Health Services (DHS) created a COVID-19 Patient Facing Communication Committee in March 2020. The goal was to provide vital information to DHS and My Health LA patients on topics such as staying safe, reducing the spread of COVID-19 and accessing care and community resources during the pandemic. The committee delivered timely information to patients through several communication tools, including text messages, robocalls, e-mails, educational videos, the MyWellness Patient Portal and a new webpage.
More than four million text messages, emails, and robocalls were sent. The coordinated communication efforts, produced in partnership with DHS leadership, targeted some of the most vulnerable residents of Los Angeles County. The committee shared critical information about COVID-19 through culturally and linguistically tailored messaging. The messages also reinforced the work of County agencies (DHS, Department of Public Health, Department of Mental Health) to help our patients learn how to protect themselves and others. The committee measured the effectiveness of the outreach through website visitor volume, number of videos played, and click-through rate to the webpage.

COVID 19 Nurse Advice Line
COVID-19 came unexpectedly into our lives and the world causing fear, confusion and uncertainty. As infection and death rates increased in Los Angeles County, so did questions from DHS patients about what to do and where to get help. A decision was made by the Department of Health Services’ (DHS) leadership to rapidly create and launch a 24-hour-a-day, 7-day-a-week COVID Nurse Advice Line (CNAL), where DHS patients could have their questions and concerns about COVID-19 quickly addressed by a nurse.
Staff from the Office of Patient Access (OPA), Population Health Management and the Ambulatory Care Network (ACN) quickly coordinated with nursing leadership to reassign and train seventeen Registered Nurses (RNs) to participate in the CNAL. Within a couple weeks, DHS leadership developed and implemented a plan for a remote call center, including developing training materials for the RNs on COVID 19 advice procedures. On April 3, 2020 DHS launched the DHS COVID-19 Nurse Advice Line. In doing so, the CNAL has successfully prevented a flooding of DHS primary care clinics and emergency rooms with questions or medical concerns that can be handled by a nurse by phone.
COVID-19 Protocol Training Using Microsoft Teams
The Department of Health Services (DHS) has identified an urgent need to expand COVID-19 testing to patients at every clinic and hospital in the DHS network. However, testing patients for COVID-19 is not a simple process; much training is required. Nursing leadership from Population Health and the Ambulatory Care Network (ACN) worked in coordination with the DHS Outpatient Care Interdisciplinary Practices Committee (DHS OP IDPC) to develop and implement Standardized Procedures/Protocols (SPSPs) for Registered Nurses (RNs), Licensed Vocational Nurses and Certified Medical Assistants.
The SPSPs for COVID-19 test ordering created a process by which licensed and certified staff could safely, efficiently and effectively expedite COVID-19 testing for patients while allowing providers to focus on seeing their COVID-19 and non-COVID patients. In “normal” times, SPSP training is provided to staff in a classroom style setting at DHS’s health facilities on different days. However, with COVID-19 requiring that SPSPs be implemented urgently, and with social distancing rules making in person trainings impossible, trainings were immediately rolled out on the new Microsoft TEAMS platform. Over 600 employees were trained on the new testing procedures in just eight days.
High Risk Patient Follow Up During COVID-19
The pandemic has led some patients to delay essential care out of fear that visiting their healthcare provider might expose them to COVID-19. The decision to postpone care comes with serious health implications for high risk patients living with chronic diseases, potentially resulting in complications or death. When the pandemic hit, DHS hospitals experienced a significant drop in non-COVID-related emergency room visits and primary care teams were concerned that high-risk patients might “fall through the cracks” and not present for care. In response, DHS Population Health leadership coordinated system-wide outreach for high-risk patients.
Patients with diabetes, hypertension, asthma, depression, substance use and other chronic conditions who had not had a primary care visit since March 15, 2020 were called to see how they were doing and if they had any unmet needs. Nurses, Medical Assistants, Patient Access Center and Social Work staff across sites made 1,600 outreach calls – over 700 patients were contacted, and more than 300 appointments were scheduled. Patients’ needs were also met by refilling medications, referring to specialty care providers, and connecting patients to Social Work to assist with housing, food, and other social needs.
HPV Vaccination Improvement
Prior to the pandemic, Drs. Stacy Barron (OV), Amy Shekarchi (OV), Raymond Perry (Humphrey), Eric Fein (Harbor), and Niloufar Tehrani (Harbor) received a grant from the American Cancer Society (ACS) to increase Human Papillomavirus Infection (HPV) vaccination rates across Los Angeles County. During the pandemic, the team has doubled vaccine initiation rates in the three sites’ nearly 2,000 empaneled pediatric patients.
Now almost half of all empaneled patients eligible for the first dose of HPV vaccine have received it. The team also increased vaccine series completion by ten percent. Through their collaborative work with the Department of Public Health and multiple Department of Health Services (DHS) committees, the team also helped revise DHS’ HPV vaccination best practices, proposed lowering the age for vaccine initiation to 9 years to the standardized procedure committee (in alignment with Centers for Disease Control recommendations), and hosted virtual learning sessions on HPV vaccinations for faculty and staff across sites. In the next phase of their project, the team will provide transportation assistance in the form of gift vouchers to patients who are due for HPV vaccination or who are receiving cancer treatment at one of the three DHS facilities.

MLK Outpatient Going Beyond Food Distribution
As the pandemic settled into Los Angeles, the staff at Martin Luther King (MLK) Outpatient Center noticed that referrals for food distribution increased by nearly 200 from May to June. “They were new to the hard times,” said Lalee Vicedo, a supervisor for the social work team for MLK Outpatient. The staff at MLK wanted to make sure that families had access to food and other things and to make sure that people who qualified for CalFresh and SSI would be able to access other programs.
“As a result, we launched a small food distribution program partnering with local nonprofits in South LA that work with small farmers in South LA like the Village Market to supply these families with local, fresh food,” said Vicedo and they also wanted to provide patients with a thorough screening for all their needs. They assessed their food and other needs and provided resources for them. They would then refer patients based on their needs to other departments i.e., to the medical/legal partnership team, housing services etc. For Vicedo, highlighting social needs and making sure that partners know that those are intertwined with medical care is essential

Olive View Pediatric Well Child Care and Vaccinations
The Pediatric Primary Care Clinic relocated twice to new physical locations to improve workflow and better meet the needs of the patients. Despite having the challenges of relocation and the pandemic resulting in less face to face visits, the clinic has maintained excellent care of its patients! The clinic team worked together to quickly transition face to face visits to phone provider visits and maintain the same number of appointments. Children needing vaccines and growth measurements are given a separate nurse visit prior to the phone visit with the provider so that providers can give adequate counseling and guidance over the phone.
Through these efforts, and with significant support from hospital administration, the clinical team has maintained its pre-COVID visit volume of 200-300 visits per week, reduced No Show rates from 30-40% pre-COVID to 10-30% post-COVID by maintaining the clinic’s usual extended hours to improve patient access, even if by phone only. Even with our moves and reduced face to face visits, our empaneled patients have been able to find and access care—our patient vaccination rates have stayed between 50 and 60% despite, according to the Centers for Disease Control, a national decrease in vaccine rates to between 40 and 50%.

Ortho Docs At Harbor Help to Prone COVID Patients
Responding to a need for innovative solutions for problems arising from the Novel Coronavirus, Dr. Louis Kwong volunteered his department to assist in putting patients in the ‘prone’ position. When patients are infected with COVID-19 and they have to be intubated, turning them in the prone position has a very effective chance at preventing mortality because there is better oxygenation in their stomachs. This wasn't a benign thing - the emergency department was in need of support and proning would reduce devastating rates of mortality. “Doing this would've exposed us to more harm, yet it was important,” says Dr. Kwong, chair of the department.
“It can be very difficult to turn a patient and if done improperly can harm the patient, even damaging their spine.” There were 26 members of the department who volunteered along with Dr. Kwong, providing a service to the patients and sparing Intensive Care Unit (ICU) nurses from potential injury. This unquestionably brought people together each day.” The ICU nurses were also very appreciative and would help the orthopedic doctors by giving them clean face shields and other personal protective equipment. The two departments also developed a closer relationship and developed a greater appreciation and respect for each other, breaking down silos in the hospital.
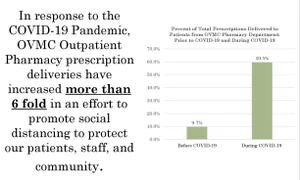
Outpatient Rx: Reduce Exposure, Improve Adherence
With the COVID-19 pandemic, Olive View Medical Center Outpatient Pharmacy redesigned the way we provide service to patients to reduce exposure while improving medication adherence. To improve patient outcomes, we had two main goals: to keep patients at home, and when patients did come to the Medical Center, to reduce the amount of time spent at the pharmacy. We first focused on mailing as many prescriptions to patients at home as possible. We encouraged patients who came to the pharmacy to sign up for the mail service and called patients who had medication refills coming up soon. We increased our in-house mail delivery 6-fold from baseline to present.
For urgent medication needs, we have started utilizing a same-day courier service and have sent over 250 deliveries to patients’ homes. For refilled prescriptions, we have significantly increased the number of prescriptions that are mailed to patients from our off-site filling facility. From a baseline of 9.7% of our total prescriptions in January and February, we increased to 59.5% in May and June. With increased call volume, we scheduled more staff to answer phones; we established a new line and voicemail just for discharging patients.

OVMC Customer Satisfaction During COVID 19
Outpatient Phlebotomy conducts a customer satisfaction survey every two years to monitor and continually strive to improve service and patient satisfaction. During the pandemic, the section implemented social distancing in the patient waiting areas and the staff work areas and educated staff on appropriate personal protective equipment (PPE). Despite the restrictions and challenges posed by the COVID pandemic, the survey written in both English and Spanish, came out with excellent results, with overall patient experience at 4.98* (in a 5-star rating scale). The survey questions were tailored to address safety during the pandemic, conducted in five days with 57 patients participating.
The following six questions were included in the survey form: [1] Was the front desk clerk courteous 4.95*, [2] Courtesy or overall experience with phlebotomist 5*, [3] Was the work area clean & sanitized 4.98*, [4] Was social distancing observed 91.2% (Yes/No), [5] Staff who drew blood were wearing the appropriate PPE 94.73% (Yes/No), [6] Overall experience 4.98*. Notable patient comments were: Good; Very friendly and nice experience; Excellent; Nice and helpful; Efficient; Very easy & helpful; Perfect!

OVMC Temporary Child Care
In response to employee childcare needs during the COVID 19 crisis, Olive View Medical Center established a temporary childcare (TCC) and enthusiastic employees from the Rehabilitation Services, Volunteer, Nursing and Communications Departments stepped up to the challenge and volunteered to staff the TCC. Many of them had no teaching or childcare background, however they possessed exceptional levels of emotional intelligence, patience, and creativity which made them an integral part of the success of this impromptu day care.
The TCC allowed their colleagues to continue to provide the necessary services our community needed. Most of them were not sure of what to expect, but their creative minds came up with ideas to keep the kids safe, engaged, and entertained during their stay at the day care. Staff were willing to shift their schedules to ensure all kids/families were accommodated. Every time staff reported back to their regular work, they’d have exciting stories to tell about their new-found vocation. It was evident in their spirits that they cared for their new young friends. This project is still on going and many staff have returned to their normal duties in the hospital. But if called again, without hesitation, the team is ready to assist in anyway.

Pediatric Nurses at LAC+USC Now Serving All Ages
The nursing staff from the Pediatric Intensive Care Unit (PICU) at LAC+USC deserves recognition for the way they have adapted to different responsibilities they needed to take on during the pandemic. The PICU department staff have had to re-train to help adults since there is a bigger need in those spaces. They all accepted the challenge and some staff members completely left the PICU to serve in departments that are needed.
The PICU staff has stepped up in a courageous manner. They have embraced the challenge to care for every age group in the entire hospital. On a daily basis, they are being floated to Neonatal Intensive Care Unit, Surgery Intensive Care Unit, Medical Intensive Care Unit, Burns Intensive Care Unit (ICU), Neuro ICU and wards. They are the only group in the facility capable of caring for every age group in this facility and have embraced this challenge beautifully. The days are often challenging and scary, but they have not hesitated providing care in areas that are unfamiliar with them. They have embraced training and education and feel blessed to have jobs at LAC+USC Medical Center. They are SUPERSTARS!
Post Hospital Follow-Up for COVID-19 Patients
Given the unpredictability of the COVID-19 disease, and with so much harm done by COVID-19 to one’s body and life, care of COVID+ patients does not end after discharge from a County hospital or ER. Leaders from DHS Population Health and the Office of Patient Access worked together to implement a new Expected Practice whereby all patients discharged with a COVID-19 diagnosis are contacted at least once, and often several times, after discharge.
Each DHS hospital created a detailed follow-up plan for their COVID-19 patients and, perhaps most remarkably, every patient is to be given a regular empaneled primary care provider and primary care medical home (PCMH) team (if they do not already have one) before they leave the hospital. Once a COVID-19 patient leaves the hospital, they receive a call from their primary care team within 72 hours. Patients are asked if they have a cough, fever, shortness of breath, chest pain or any other lingering effects of COVID-19, but they are also asked if they have access to food or have mental health or life concerns that need to be addressed while they recover. These post-discharge phone visits are essential to provide counseling and moral support to recovering patients as they try to restore their lives to normalcy.

Primary Care Drive-up Services
The World Health Organization states that during a pandemic, continued access to vaccination services is imperative to prevent concurrent outbreaks of other communicable diseases. Patients’ families at LAC+USC Medical Center were hesitant to come to our clinics to receive vaccinations for their children during the Covid-19 pandemic. To minimize exposure and risk to families, we designed a drive-up primary care service offering pediatric vaccinations. Patients are scheduled for an appointment, are greeted curbside by a clinic team member, and remain in their vehicle during the visit.
Additionally, we know that the economic devastation caused by Covid-19 disproportionately impacts the patients and families in our care. Therefore, those who screen positive for food insecurity are met with a box of fresh and non-perishable food at the curb when they arrive for their drive-up appointment. To date, the drive-up clinic has vaccinated over 110 children. One-third of families coming to the drive-up vaccine clinic have received food distribution due to food insecurity. We have received positive feedback from families, who noted that the visit was "quicker than coming to the clinic building" and they "felt safe coming to the drive-up clinic" for vaccines.

Psychological Support at LAC USC
When the pandemic started ramping up, the department of Psychiatry at LAC+USC Medical Center, sensing the weight of this challenge, put together a grand rounds series with the whole department to figure out what role the mental health providers could play in the crisis. There were a lot of reports of front-line health workers at the hospital feeling high levels of burnout because of the stress due to working during the pandemic so Jordan David, resident psychiatrist in the LAC+USC Department of Psychiatry decided to work with Tobi Fishel, head of GME Wellness and the leader of the Health and Healers Heal (H3) program and quality control officer, Laura Sarff to do something.
The outcome: resident physicians in the LAC+USC Department of Psychiatry conceived of, designed, and implemented a volunteer peer support hot line to support all medical center staff who have been impacted by the COVID-19 pandemic. Staff were provided a 30-minute conversation with a mental health provider to help deal with stress by speaking to someone who knows something about what they are going through.

Rancho Employee Childcare-We Are Family
During the pandemic, Rancho leadership has continued to show its strength by looking out for its ‘family’ of patients and employees. Rancho recognized the challenges many staff were encountering as school moved to virtual learning and parents were still trying to come to work. Rancho, in collaboration with Don Knabe Wellness Center (DKWC)/Rancho Research Institute and Rancho Los Amigos Foundation (RLAF), opened the Rancho Employee Childcare Center in late March 2020. Staffing was a kaleidoscope of Rancho clinical staff, Rancho KnowBarriers peer mentors, and disaster service workers from across Los Angeles County.
Children attended the childcare in the DKWC building, with craft supplies and snacks provided by RLAF. Childcare staff and children alike enjoyed our beautiful new outdoor campus; especially the weekly visits to the Rancho Therapeutic Garden. We made cardboard cars, celebrated a couple birthdays, made Rancho Hero posters to celebrate our staff and even created a YouTube video reminding us all to wash our hands and stay six feet apart. Rancho is grateful to the Los Angeles County family for providing us with the extra staffing we needed to provide this service to our employees!

Rancho Expands Telehealth Services
The COVID-19 stay-at-home order threatened the sense of community our patients enjoy at the Rancho Los Amigos National Rehabilitation Center (Rancho). In response, the Ambulatory Care leadership team immediately committed to expanding our telehealth services. In 2019, we averaged 165 telehealth visits per month. After pausing most in-person visits in March 2020, we averaged 400+ telehealth visits per week. Therapy and mental health providers started utilizing telehealth visits. We experienced a new commitment to work as a team to increase the number of patients enrolled and utilizing the MyWellness Patient Portal.
Rancho also wanted to enhance its current telehealth services by developing video telehealth visits via Zoom. The team created practice sessions between a KnowBarriers peer mentor and providers. The experience led to a new workflow utilizing clinic support staff, messaging utility, and Zoom. Today we are beginning to offer video telehealth visits in select clinics. Patients who are interested in a video telehealth visit are offered a video telehealth ‘video test call’ with a peer mentor. The peer mentor has a checklist of tasks to practice with the patient and provide feedback to the provider prior to the telehealth video visit. We are excited to expand & enhance our telehealth services for our patients.

Rancho Finding New Solutions During Pandemic
The team at Rancho Los Amigos National Rehabilitation Center (Rancho) discovered that sick patients recovering from COVID-19 couldn't do things that they used to be able to do – leading them to pull together a new service line for people who had been through COVID-19 and needed rehabilitation. The Rancho COVID-19 rehab team developed a database early on to collect information and track outcomes (ex. how well patients are able to function, how well patients were when they left), so that they could share best practices with the rehab community across the country.
“Innovation was a huge part of success in dealing with the pandemic,” said Michael Scott, Physician at Ranchos. The team also figured out how to do their jobs from a distance, using a video medical interpretation system, and found new ways to get the patients out of the room safely on short notice and in a very collaborative way. Physicians, speech and occupational therapists, psychiatrists, social workers and case managers all came together in a team effort, and the collaboration of the team was integral to every success story.

Rancho Provides Virtual Support During Pandemic
At the onset of the ‘stay at home’ order, Rancho recognized the potentially devastating impact to the large number of outpatients who utilize the many services at Rancho to meet their needs of community. The Rancho KnowBarriers Peer Mentor service stepped up to provide our existing support groups virtually. This was no small task! Establishing a Zoom account, coordinating with the various Peer Mentor support group facilitators to determine potential participants, and develop a system to help participants and facilitators adapt to using Zoom.
Keep in mind that many of the peer mentor facilitators and participants are recovering from a stroke or acquired brain injury; many have limited experience and access to technology. Today we host 9 weekly support groups, in English and Spanish languages, averaging over 100 participants per week! One man joins us from Colorado. The support groups are invaluable to share COVID related benefit programs, testing information, and provide the ‘Rancho community’ support our patients rely on. We would like to acknowledge Rancho Psychology and the Don Knabe Wellness Center/ Rancho Research Institute for partnering with us to provide Virtual support to our patients.
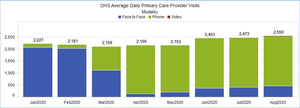
Rapid Transition to Telehealth During COVID-19
The COVID-19 pandemic has ushered in a period of unprecedented and rapid change in how we serve our patients at the Los Angeles County Department of Health Services (DHS). Before COVID-19, over 90% of our patient-provider visits were conducted in-person. By April, we had flipped the paradigm, with 90% of our patients now seen through telehealth encounters. Most of those patient visits were done by phone, utilizing adult and pediatric guidelines for how to conduct team-based provider phone visits. We have also ramped up our capacity to do video and drive-through visits at the same time.
In doing so, we haven’t just maintained access to care for our patients during this crisis, we’ve increased it: the average number of provider visits per day is now up compared to pre-COVID-19 benchmarks. As we shift our approach to serving patients, DHS has created new guidelines for providers on how they can best conduct team-based telehealth visits. It’s part of a broader effort within DHS to use the renewed sense of urgency and mission unleashed by this pandemic to rethink how we can best serve the changing needs of our patients amid a dramatically altered health care landscape. Telehealth has become a critical tool of care during the pandemic, and will certainly continue to be important after the pandemic has ended.

Safe @ Home O2 Program
To mitigate the risk of preventable mortality and optimize access to acute care during the Covid-19 pandemic, the Department of Health Services issued an expected practice whereby Covid-19 patients on low-levels of oxygen could be managed at home. Medical centers were instructed to develop their own, local processes, and LAC+USC Medical Center developed the SAFE @ HOME O2 Program. The program launched on April 3rd, and through mid-July it enabled over 400 patients to return home on oxygen. No patients died at home, no patients died in the field, and no patients died after leaving the ED with oxygen.
The few deaths that were observed occurred after return hospitalizations, with a resulting all-cause mortality of less than 1.5%. Readmission rate within 14 days of discharge was only around 10%, indicating that the program was overwhelmingly effective in preserving acute care access during the pandemic. Finally, patients reported positive experience with the program. Please refer to links below for further information on patients’ experiences.
Patient Education Video: https://lacusc.live/SafeAtHome
Administrative Briefing Video https://vimeo.com/444725266/fff50b538c

Strong Healthy and Resilient Kids (SHARK) Program
Through a multidisciplinary Olive View-UCLA, Rancho Los Amigos, and Ambulatory Care Network partnership, the Strong Health and Resilient Kids (SHARK) program launched in May 2020 to promote resilience and needed service linkages for children and families receiving care across Los Angeles County Department of Health Services. The program, through partnerships with First 5 LA and other community organizations, provides early screening and intervention services to children experiencing toxic stress in the setting of developmental, behavioral, mental health, and/or social needs.
Clinicians from across Los Angeles County can consult the SHARK team for assistance in management or service linkage for their patients. In addition to consultative services, the SHARK program offers a Primary Care Medical Home to pediatric patients with complex care needs and a multidisciplinary team-based inpatient service. With its launch at the start of the pandemic, the SHARK team—three pediatricians, a family medicine physician, a mental health clinician, physical therapist, occupational therapist, and social worker—has served many patients through telehealth visits.
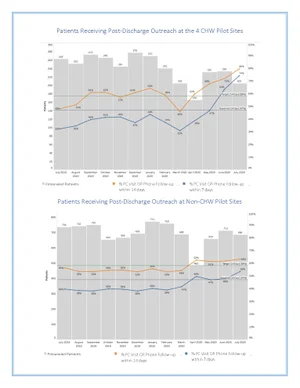
TOC Post-Discharge Call Pilot Using CHWs
Transitioning from the hospital to home is a known high-risk transition period that can be associated with adverse patient outcomes including readmission. Performing timely outreach to recently discharged patients is a best practice and a National Committee for Quality Assurance requirement. However, this can be challenging during the pandemic when there are additional clinical priorities. Four Whole Person Care (WPC) Community Health Workers (CHWs) were assigned to Department of Health Services (DHS) primary care medical homes that had COVID-related staff redeployments.
Partnering the WPC CHWs with nursing, we developed a workflow for the CHWs to perform Transitions of Care post-discharge phone calls to recently discharged DHS-empaneled patients. The CHWs identified patients from a custom report and called them utilizing a phone script that has escalation pathways to nursing, pharmacy, scheduling and/or social work. The CHWs documented in Online Real-time Centralized Health Information Database and coordinated follow-up with multi-disciplinary team members. By the second month (July 2020) of the pilot, 74% of recently discharged patients received outreach within 7 days, up from a nadir of 31%. Given the success of this pilot and the valuable role that CHWs can play in post-discharge support, we plan to expand to additional sites.